When you have a virus, it’s not actually the virus that makes you sick, but your immune system’s efforts to get rid of it. For example, your immune system can raise your body temperature and give you a fever, to make it hot enough to kill a virus. All the hard work your immune system is doing can also use up energy and make you feel tired.
Everyone’s body is different, and because symptoms are caused by your immune system and not the virus itself, different people can have slightly different symptoms when they have the same virus, and some people’s symptoms will be worse than others.
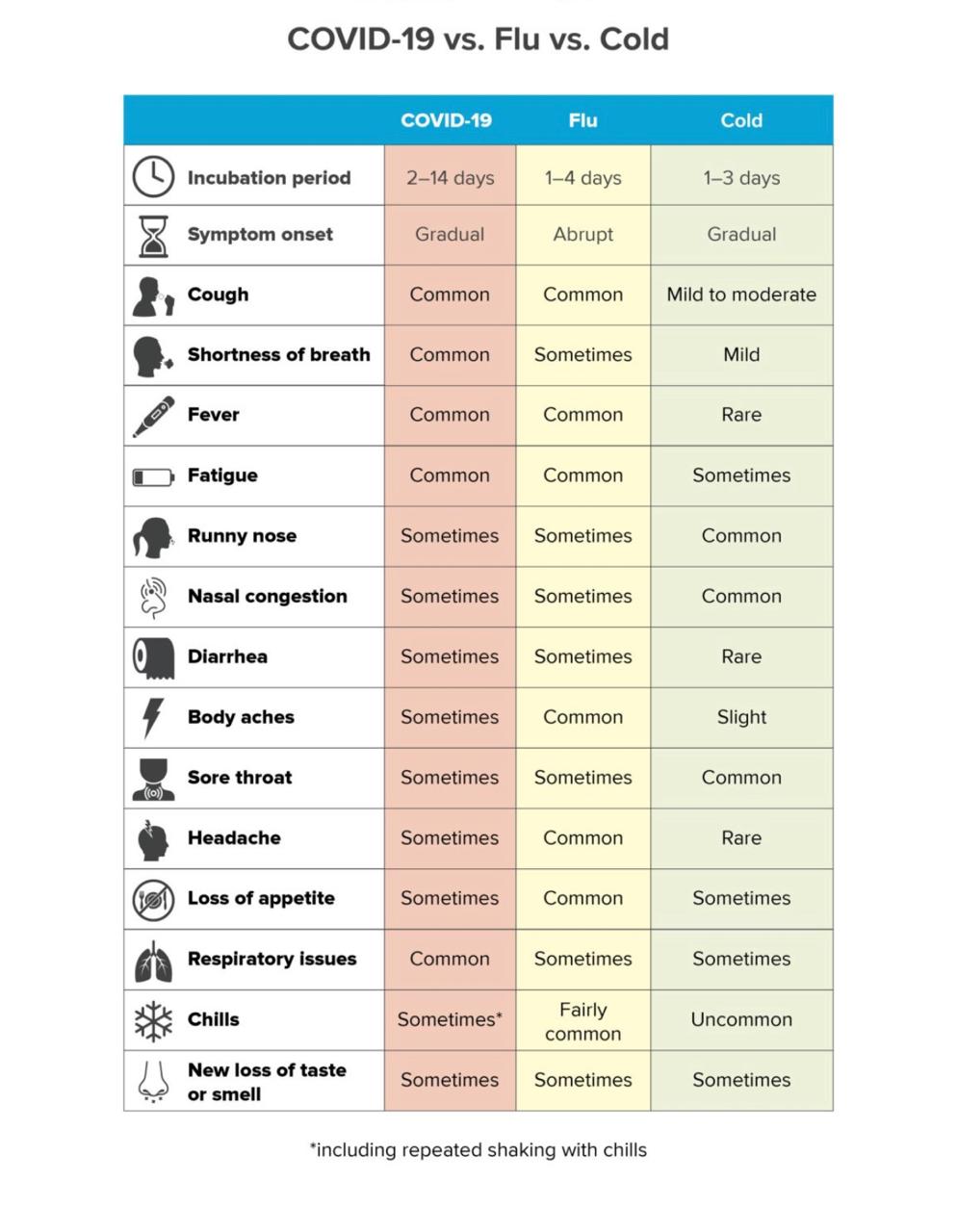
COVID-19 is a respiratory illness, which means it affects the parts of your body you use to breathe: your nose, throat and lungs. If you’re sick with COVID-19, your symptoms might include:
1.fever
2.a cough
3.sore throat
4.fatigueshortness of breath
5.runny noseloss of smell and/or taste
6.Few people also have Diarrhea , abdominal discomfort and vomitings ( rarer symptoms)
Symptoms may develop 2 days to 2 weeks following exposure to the virus.
A research analysis of confirmed cases of COVID-19,found the mean incubation period to be 5.1 days and that 97.5% of individuals who developed symptoms did so within 11.5 days of infection
When you look at the virus through a microscope, coronaviruses look kind of like a crown. Corona means crown in Latin, which is how coronaviruses got their name.
At first, we called this virus ‘novel coronavirus’, which means a new strain of coronavirus. Once scientists figured out exactly what this strain of coronavirus was and how to identify it in tests, they gave it a name: SARS-CoV-2.
When someone gets sick with this virus the illness is called COVID-19. For simplicity, a lot of people are calling the virus and the disease it causes the same name, COVID-19.
A small number of pets worldwide, including cats and dogs, have been reported to be infected with the virus that causes COVID-19, mostly after close contact with people with COVID-19. Based on the limited information available to date, the risk of animals spreading COVID-19 to people is considered to be low.
It appears that the virus that causes COVID-19 can spread from people to animals in some situations.
Treat pets as you would other human family members – do not let pets interact with people outside the household.
If a person inside the household becomes sick, isolate that person from everyone else, including pets.
This is a rapidly evolving situation and information will be updated as it becomes available.
Study of positive coronavirus cases in two of the worst affected countries, China and Italy points to somewhat selective pattern of the spread of Covid-19. That the novel coronavirus targets the older people and avoids the young ones.The 10-19 age group formed just one per cent of total novel coronavirus infection. Those below 10 comprised had a less than one per cent share. No death has been reported in the age group.
This does not mean that children are completely immune to novel coronavirus infection. In China and the UK have reported about newborns having tested positive for novel coronavirus. Though, the disease Covid-19 has not been found to be transferring from mother to child during pregnancy.
As you get older, your risk for severe illness from COVID-19 increases. For example, people in their 50s are at higher risk for severe illness than people in their 40s. Similarly, people in their 60s or 70s are, in general, at higher risk for severe illness than people in their 50s. The greatest risk for severe illness from COVID-19 is among those aged 85 or older.
There are also other factors that can increase your risk for severe illness, such as having underlying medical conditions diabetes, heart disease, hypertension, obesity etc .By understanding the factors that put you at an increased risk, you can make decisions about what kind of precautions you have to take in your daily life.
But the fact that children are largely untested underscores that they can be carriers or vectors of novel coronavirus. Also, medical conditions like asthma and diabetes are not uncommon among children. In many cases obesity-linked diabetes and asthma are related. In such cases, novel coronavirus infection can be fatal for children also.
Respirators
Fit- and seal-tested respirators are made of tangled fibers that are highly effective at filtering pathogens in the air. These respirators must meet the rigorous filtration standards set by the National Institute for Occupational Safety and Health (NIOSH).
The diameter of the coronavirus is estimated to be 125 nanometers (nm). Keeping this in mind, it’s helpful to know that:
Certified N95 respirators can filter 95 percent of particles that are 100 to 300 nm in size. N99 respirators have the ability to filter 99 percent of these particles. N100 respirators can filter 99.7 percent of these particles.
Some of these respirators have valves that allow exhaled air to get out, making it easier for the user to breathe. However, the downside of this is that other people are susceptible to the particles and pathogens that are exhaled through these valves.
Surgical masks
There are various types of surgical masks. Typically, these disposable, single-use masks are cut into a rectangle shape with pleats that expand to cover your nose, mouth, and jawline. They are composed of breathable synthetic fabric.
Unlike respirators, surgical face masks don’t have to meet NIOSH filtration standards. They aren’t required to form an airtight seal against the area of your face that they cover.
How well surgical masks filter pathogens varies widely, with reports ranging from 10 to 90 percent.
Despite differences in fit and filtration capacity, a randomized trial found that surgical face masks and N95 respirators reduced participant risk of various respiratory illnesses in similar ways. Adherence or proper and consistent use played a more pivotal role than the type of medical-grade mask or respirator worn by study participants.
Cloth masks
Do-it-yourself (DIY) cloth masks are less effective at protecting the wearer because most have gaps near the nose, cheeks, and jaw where tiny droplets can be inhaled. Also, the fabric is often porous and can’t keep out tiny droplets.
Although cloth masks tend to be less effective than their medical-grade counterparts, experimental results suggest they are far better than no mask at all when worn and constructed properly.
Any regular soap what you have been using would suffice to wash your hands the main aim is to keep your hands clean.
A good quality alcohol based sanitiser usually doesn’t cause allergic reaction Alternatives are spirit, u can make a sanitiser with isopropyl alcohol ,glycerol at home.
Accumulating evidence supports ending isolation and precautions for persons with COVID-19 using a symptom-based strategy. Specifically, researchers have reported that people with mild to moderate COVID-19 remain infectious no longer than 10 days after their symptoms began, and those with more severe illness or those who are severely immunocompromised remain infectious no longer than 20 days after their symptoms began. Therefore, CDC has updated the recommendations for discontinuing home isolation as follows:
Persons with COVID-19 who have symptoms and were directed to care for themselves at home may discontinue isolation under the following conditions:
1. At least*10 days* have passed since symptom onset and At least 24 hours have passed since resolution of fever without the use of fever-reducing medications and Other symptoms have improved.
2. A limited number of persons with severe illness may produce replication-competent virus beyond 10 days, that may warrant extending duration of isolation for up to 20 days after symptom onset.
3. Consider a consultation with infection control experts before discontinuing home isolation .( here u can put a direct active link to book online physician consult at SHC)
4. Persons infected with SARS-CoV-2 who never develop COVID-19 symptoms (Asymptomatic positive)may discontinue isolation and other precautions 10 days after the date of their first positive RT-PCR test for SARS-CoV-2 RNA.